About the OCAD Calculator
Information
The CT calcium score scan is not indicated as the initial investigation in patients with:
- typical angina pectoris symptoms.
- additional other cardiac symptoms, such as exertional dyspnea suggesting heart failure or pulmonary disease, palpitations, or suspected valvular disease. In these cases, referral to secondary care is advised.
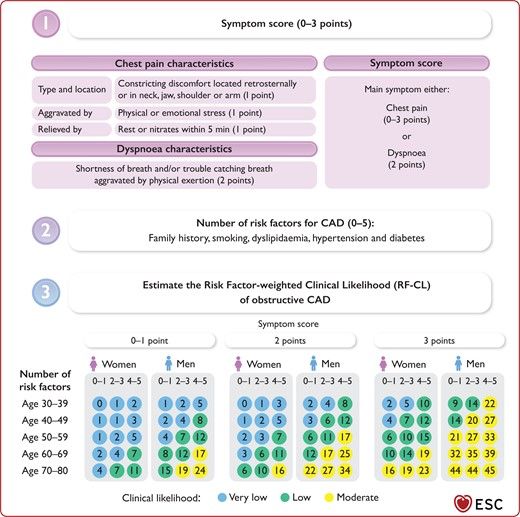
The pre-test probability of obstructive coronary artery disease is determined using the “risk-factor-weighted clinical likelihood model” (RF-CL model) (see table in the Rationale). This model is based on the following data: type of thoracic symptoms, age, sex, and the presence or absence of diabetes, hypertension, dyslipidemia, (previous) smoking, and family history (first-degree relatives with coronary artery disease at a young age, i.e., men <55 years and women <65 years).
In which patients is the CT calcium score scan not indicated?
Caution is advised when requesting a CT calcium score in patients with: thoracic symptoms and a potentially higher cardiovascular risk profile than calculated with the RF-CL model due to risk factors that are not part of the RF-CL model, such as familial hypercholesterolemia, severe renal impairment, autoimmune diseases, or peripheral arterial disease.
Footnote
The clinical likelihood of obstructive CAD should be estimated based on the RF-CL model (figure 1). Individual adjustment of the RF-CL values is in some cases needed based on abnormal clinical finding (figure 2) or highly suspicious symptoms. Beyond the CACS-CL no methods are validated to give accurate adjusted values to the RF-CL and the adjusted values is therefore based on clinical judgment.
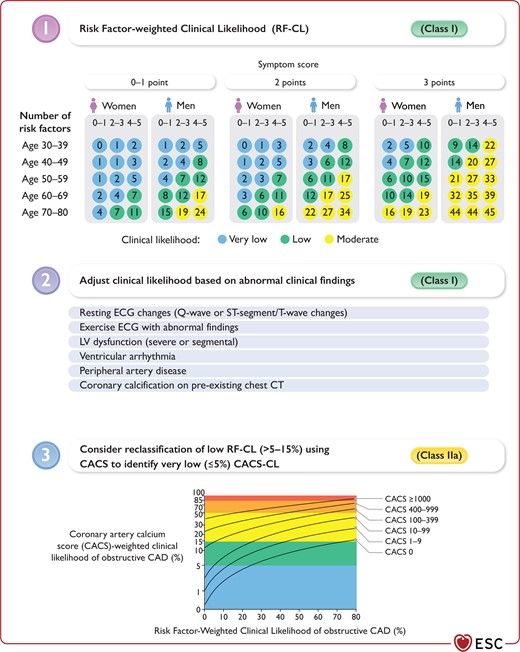
Background
In general, individuals with a very low (≤5%) likelihood of obstructive CAD do not require further diagnostic testing unless symptoms persist and non-cardiac causes have been excluded. In patients with a low (>5%–15%) likelihood of obstructive CAD, the benefit of diagnostic testing is uncertain but may be performed if symptoms are limiting and require clarification. Patients with moderate (>15%–50%), high (>50%–85%), and very high (>85%) likelihood of obstructive CAD are encouraged to undergo further diagnostic testing.
Individual adjustment of the likelihood may be necessary for individuals with severe single risk factors or comorbidities associated with an increased prevalence of obstructive CAD, which are not reflected in the RF-CL model, e.g. familial hypercholesterolaemia, severe kidney dysfunction, rheumatic/inflammatory diseases, and peripheral artery disease (PAD).
Data used
| Women | Men | Women | Men | Women | Men | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of risk factors | 0–1 | 2–3 | 4–5 | 0–1 | 2–3 | 4–5 | 0–1 | 2–3 | 4–5 | 0–1 | 2–3 | 4–5 | 0–1 | 2–3 | 4–5 | 0–1 | 2–3 | 4–5 |
| Age 30-39 | 0 | 1 | 2 | 1 | 2 | 5 | 0 | 1 | 3 | 2 | 4 | 8 | 2 | 5 | 10 | 9 | 14 | 22 |
| Age 40-49 | 1 | 1 | 3 | 2 | 4 | 8 | 1 | 2 | 5 | 3 | 6 | 12 | 4 | 7 | 12 | 14 | 20 | 27 |
| Age 50-59 | 1 | 2 | 5 | 4 | 7 | 12 | 2 | 3 | 7 | 6 | 11 | 17 | 6 | 10 | 15 | 21 | 27 | 33 |
| Age 60-69 | 2 | 4 | 7 | 8 | 12 | 17 | 3 | 6 | 11 | 12 | 17 | 25 | 10 | 14 | 19 | 32 | 35 | 39 |
| Age 70-80 | 4 | 7 | 11 | 15 | 19 | 24 | 6 | 10 | 16 | 22 | 27 | 34 | 16 | 19 | 23 | 44 | 44 | 45 |
Clinical likelihood (in %)
Very low pre-test probability of obstructive coronary artery disease. Recommendation: no additional CT calcium score necessary, as this will not further reduce the probability.
If symptoms persist, consider angina with non-obstructive coronary artery disease (ANOCA).
Moderate pre-test probability of obstructive coronary artery disease. Recommendation: consider CACS for further risk stratification.
Higher pre-test probability of obstructive coronary artery disease. Recommendation: refer for diagnostics in secondary care.
References
- Vrints C, et al. 2024. 2024 ESC Guidelines for the management of chronic coronary syndromes: Developed by the task force for the management of chronic coronary syndromes of the European Society of Cardiology (ESC) Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal. 2001 Jun 1;87(11):1335-9DOI | PubMed